The level of fibrinogen in the blood is directly related to the coagulation process; however, alterations in values can be associated with disease.
 The fibrinogen blood test, also known as “factor I activity,” is used to determine the levels of this substance related to clotting.
The normal level should be between 200 and 400 milligrams per deciliter (mg/dl) of blood. However, this varies somewhat with the age of the person. In fact, it is usually a little lower in children under five years of age.
However, the test results can indicate whether there is a deficiency or, conversely, a high level of fibrinogen in the blood. In turn, this increase or decrease is related to various factors, such as diseases, pregnancy, menopause, and drug use.
The fibrinogen blood test, also known as “factor I activity,” is used to determine the levels of this substance related to clotting.
The normal level should be between 200 and 400 milligrams per deciliter (mg/dl) of blood. However, this varies somewhat with the age of the person. In fact, it is usually a little lower in children under five years of age.
However, the test results can indicate whether there is a deficiency or, conversely, a high level of fibrinogen in the blood. In turn, this increase or decrease is related to various factors, such as diseases, pregnancy, menopause, and drug use.


 The fibrinogen blood test, also known as “factor I activity,” is used to determine the levels of this substance related to clotting.
The normal level should be between 200 and 400 milligrams per deciliter (mg/dl) of blood. However, this varies somewhat with the age of the person. In fact, it is usually a little lower in children under five years of age.
However, the test results can indicate whether there is a deficiency or, conversely, a high level of fibrinogen in the blood. In turn, this increase or decrease is related to various factors, such as diseases, pregnancy, menopause, and drug use.
The fibrinogen blood test, also known as “factor I activity,” is used to determine the levels of this substance related to clotting.
The normal level should be between 200 and 400 milligrams per deciliter (mg/dl) of blood. However, this varies somewhat with the age of the person. In fact, it is usually a little lower in children under five years of age.
However, the test results can indicate whether there is a deficiency or, conversely, a high level of fibrinogen in the blood. In turn, this increase or decrease is related to various factors, such as diseases, pregnancy, menopause, and drug use.
Contents
What is fibrinogen, and what is its function?
There has always been great interest in understanding coagulation. In ancient times, this process was thought to be due to solidification by cooling. At the beginning of the 20th century, with the publication of a study by Paul Morawitz, research in this regard is refocused. Fibrinogen, or Factor I, is a protein synthesized in the liver and incorporated into the blood plasma. It is part of the group of coagulation factors, along with prothrombin, calcium, and tissue factor, among others. There are 13 in all. Therefore, it is responsible for stopping bleeding when there is a wound or hemorrhage. This complex process is known as “hemostasis” or “clotting cascade.” During it, thrombin helps to convert fibrinogen into fibrin, which works like cement and forms a mesh or network. In turn, the platelets stick together—like bricks—to produce a clot that plugs the wound. In the opposite process, fibrinolysis, fibrin activates a clot-breaking enzyme (called plasmin), and fibrinogen inhibits it. In this way, it is ensured that everything happens in an ideal way; clots break down when they are no longer needed and are not formed unnecessarily. As some know, clots can be harmful; if they block blood vessels, they will lead to a heart attack or stroke. Therefore, the balance between blood fibrinogen and fibrin is paramount. In addition, fibrinogen is considered to bind and activate white blood cells, thus playing an important role in the immune response to infection or injury. Some recent findings seem to confirm it. For example, in an investigation of patients presenting with sepsis, rapid recovery and lower mortality were correlated with increased fibrinogen. Another laboratory study conducted on mice suffering from acetaminophen-induced liver damage found that fibrinogen can help repair the liver by activating white blood cells.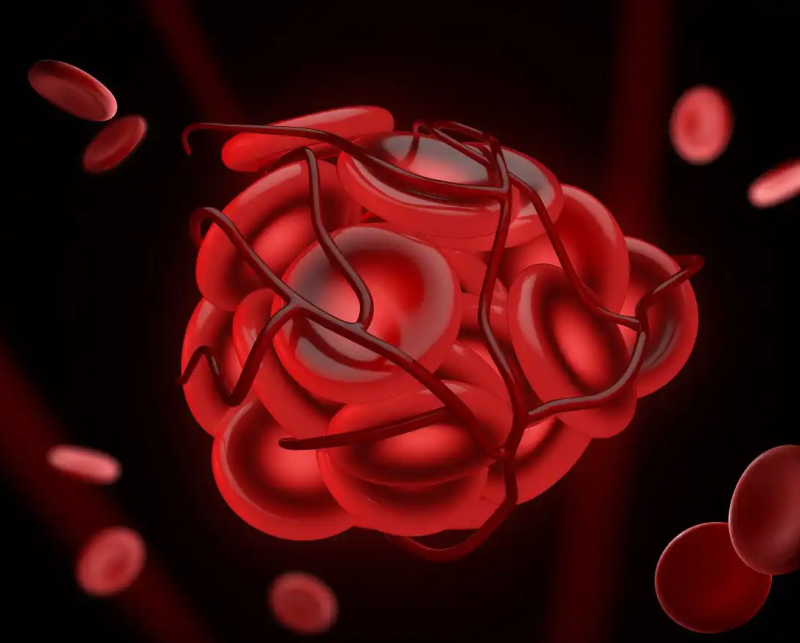
How and for what is the fibrinogen blood test done?
The fibrinogen blood test is done to estimate how well the clotting process is working. Often, it is suggested to be performed while fasting for up to 12 hours. Even if special preparations are not required, the doctor may recommend that medication be stopped in advance, especially if it is an anticoagulant. A serum sample is taken directly from the vein (it can be ulnar or cephalic) with a syringe to carry out the test. The needle is withdrawn when enough blood (approximately two ccs) has been drawn. Then, a standard amount of thrombin is added to the sample, and the time it takes for the fibrin clot to form is measured. This makes it possible to determine the amount, but not the activity, of fibrinogen in the blood. Said period is directly proportionally correlated with the amount of active fibrinogen in the sample. Therefore, prolonged clot formation may be due to decreased fibrinogen concentrations or dysfunction.Test Risks
Obtaining a blood sample may be more difficult for some people than others. However, the fibrinogen blood test is simple, fast, and safe; It carries no risks or major side effects. You only experience mild pain with the puncture and a bruise after it. These symptoms disappear after a while (one or two days).When to do the fibrinogen blood test?
The doctor may request a fibrinogen blood test alone or as part of a series of tests for abnormal bleeding or clotting conditions. Among other circumstances, the option is considered in any of the following cases:- Frequent nosebleeds.
- Heavy menstrual bleeding.
- Presence of blood in the urine or feces.
- Abnormal bleeding in the gums.
- Gastrointestinal tract bleeding.
- Bruises for no apparent reason.
- Spleen rupture.
- Thrombosis.
- Abnormal results of prothrombin or partial thromboplastin tests.
- Disseminated intravascular coagulation symptoms.
- Abnormal fibrinolysis.
- Inherited or acquired dysfunction related to coagulation.
What do the results mean?
The expected level of fibrinogen in the blood is 200 to 400 milligrams per deciliter (mg/dl), but this can vary somewhat with age. In fact, it is lower in children under five years of age, 160 to 400 mg/dl. And in newborns or babies under one-year-old, it ranges between 80 and 90 up to 375 or 385 mg/dl. When the results are not within this range, they are considered higher or lower than expected. Let’s look at each one separately.High levels
In this case, there is the following reference scale (in adults):- 400 – 600 mg/dl (slightly high): may be due to circumstantial factors. A new weekly analysis must be carried out to see if the values return to normal.
- 600 – 700 mg (moderately high): it is advisable to consult with the doctor. If blood pressure is also elevated, the risk of stroke increases.
- More than 700 mg/dL (excessively high): High chance of clots forming that damage the heart or brain.
Low levels
There are three types of fibrinogen deficiency in the blood:- Afibrinogenemia or complete absence of fibrinogen is rare (affects one person in 2 million). Although it does not necessarily cause bleeding when it does occur, it is severe.
- Hypofibrinogenemia: low fibrinogen levels, below 200 mg/dl. It is associated with minor bleeding.
- Dysfibrinogenemia: blood levels are normal, but fibrinogen is not working properly. It causes bleeding and thrombosis. It can be congenital or acquired and affects one person in a million.
Why is fibrinogen in the blood altered?
The factor I abnormality may be temporary. In this case, possible related factors include pregnancy (conducive to the increase), menstruation, bleeding, a blood transfusion, or drug reactions. Among the drugs that alter the levels of this protein, the following are mentioned:- Oral contraceptives.
- Estrogens.
- Steroids.
- Antituberculosis.
- Antiandrogens.
- Aspirin.
- Warfarin.
- Various medications to lower cholesterol.
- Tumors.
- Severe malnutrition.
- Nephrotic syndrome.
- Inflammatory disorders (such as rheumatoid arthritis).
- End-stage liver disease.
