Various medications for sciatic nerve pain range from commonly used pain relievers and anti-inflammatories to opioids and corticosteroid injections. Of course, they should always be prescribed by the doctor.
In addition, there are other complementary measures and approaches to drugs, such as physiotherapy, local compresses, and exercises. All can be applied to help alleviate known and unwanted sciatica.
Contents
Causes and symptoms of pain in the sciatic nerve
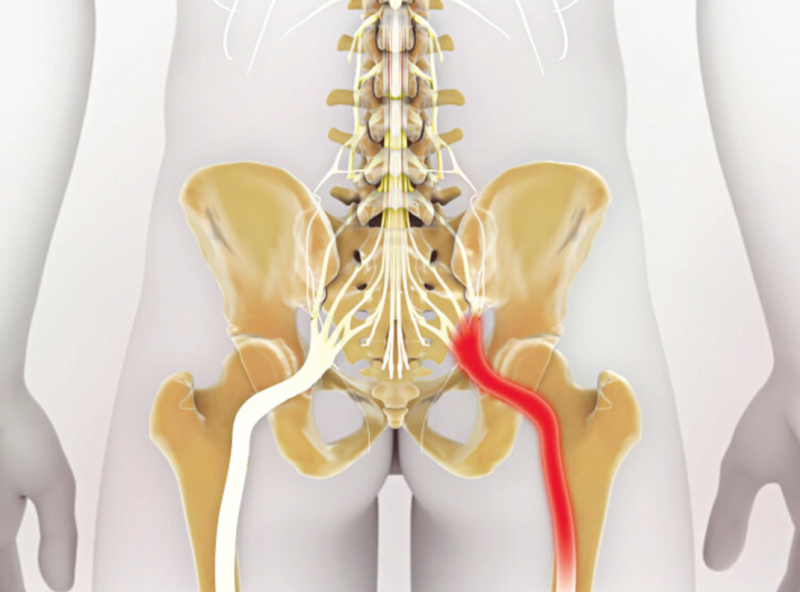
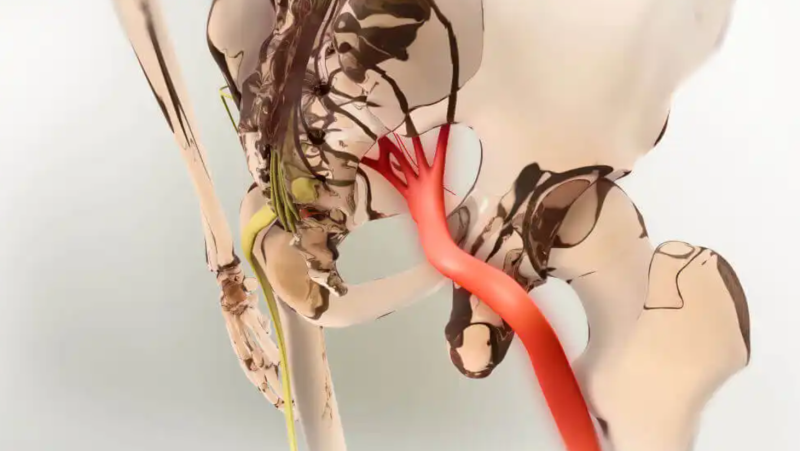
Sciatica is the pain that occurs when the nerve of the same name becomes inflamed, which, in turn, is usually the result of pinching or compression of the lumbosacral nerve roots. Possible causes include the following:
- Herniated disc.
- bone spur
- Nerve or sheath tumors.
- For example, we maintain an incorrect posture for a long time when sitting.
There are also risk factors that can predispose or trigger sciatic nerve pain. For example, jobs that require a lot of effort with the back (when carrying heavy packages) or that require us to remain seated for a long time (drivers, sewists, tailors, office staff).
On the other hand, a sedentary lifestyle, obesity, and age condition change in the spine. In particular, being overweight can increase the strain on the back. Also, diabetes is one of the risk factors since this disease increases the chances of nerve damage ( painful diabetic neuropathy ).
As for sciatica symptoms, the pain radiates along the nerve, being felt at the end of the spine (lower back), in the buttocks, or the back of the thigh. It usually affects only one side of the body.
It may be experienced as a continuous stitch or as pinpricks. In addition, it is accompanied by a sensation of heat, burning, or tingling, as well as difficulty moving the leg, walking, or keeping the back straight.
Most used medications for pain in the sciatic nerve
Pain relievers and anti-inflammatories are the first medications prescribed for pain in the sciatic nerve. Then, if it does not remit, other more powerful ones can be recommended.
1. Paracetamol or acetaminophen
Analgesics like paracetamol are among the most used for this ailment. According to studies, there is still no information about its effectiveness against sciatica, but future tests will yield new data to support or rule out this idea.
It is appropriate to note that excessive consumption of this drug can cause side effects. The most feared is drug-induced hepatitis, usually when the recommended dose is exceeded.
2. Non-steroidal anti-inflammatory drugs (NSAIDs)
Some sciatic nerve pain medications, such as ibuprofen and naproxen, are anti-inflammatory. In addition to them, it is worth mentioning diclofenac.
Thus, non-steroidal anti-inflammatory drugs (NSAIDs) have antipyretic, anti-inflammatory, and analgesic activity. This is thanks to its ability to inhibit the enzymes synthesizing prostaglandins.
According to research, possible gastrointestinal, cardiovascular, and renal complications are indicated among the effects associated with using non-steroidal anti-inflammatory drugs, so a professional must adjust the dose.
3. Muscle relaxants
There are several classes of muscle relaxants: some are spasmolytic, and others are neuromuscular blockers. Among the most used for the treatment of sciatica are the following:
- Carisoprodol.
- Methocarbamol.
- Tizanidine.
- Cyclobenzaprine
- Orphenadrine.
Its mechanism of action is proper when muscle contractures are associated with sciatic pain, but it is impractical for all patients.
4. Corticosteroids
When the pain in the sciatic nerve is very severe and disabling, to the point that the person cannot walk or stand, corticosteroid injections may be considered.
However, they are medicines for delicate use. They should only be administered by a healthcare professional.
When the doses are high, or the treatment is prolonged, adverse effects may occur :
Short term:
- Digestive bleeding.
- Fluid retention.
- It increases blood pressure.
- Humor changes.
Long-term:
- Osteoporosis.
- Muscular weakness.
- Waterfalls.
- Immunosuppression.
According to a study by the Cochrane Collaboration, the research evidence on the effectiveness of epidural steroid injections for treating lumbosacral radicular pain is still scarce, so more research is needed. There was evidence of a slight improvement in pain and disability in the short term, although it is an effect that does not seem to be maintained over time.
5. Opioids
Opioids constitute a broad group of analgesics. Signals decrease pain perception by being distributed in the blood and interacting with receptors. There are some derivatives of the poppy and other synthetics. They can be injected or administered orally; there are even patches.
Sciatic nerve pain medications include opioids such as:
- Codeine.
- Tramadol.
- Fentanyl.
There are several risks associated with its use, including drowsiness, disorientation, and decreased heart and respiratory rates. However, many of the most important complications are derived from the high risk of addiction these medications produce.
Research published in the Journal of the Spanish Pain Society explains that using these drugs to treat chronic pain in sciatica (and low back pain in general) is complex. As proof of this, emergencies related to complications from the use of fentanyl have increased considerably.
This is why opioids are generally considered the last therapeutic step for pain, requiring professional follow-up in Chronic Pain Units in various hospitals.
6. Anticonvulsants
 As a Mayo Clinic publication explains, anticonvulsants (such as gabapentin and pregabalin ) are also used to control pain. They are considered to interfere with transmitting signals sent by damaged nerves.
As a Mayo Clinic publication explains, anticonvulsants (such as gabapentin and pregabalin ) are also used to control pain. They are considered to interfere with transmitting signals sent by damaged nerves.
However, they can cause side effects, such as nausea, vomiting, drowsiness, headaches, dizziness, blurred vision, lack of coordination, and even liver damage.
A study published in Pharmacotherapy explains that it could effectively treat sciatica. To demonstrate this, the authors report two clinical cases of patients who improved their symptoms with this drug, despite having previously received more conventional drugs.
7. Antidepressants and anxiolytics
The use of antidepressants in treating sciatica is curious when their functions are unrelated. However, as one study explains, chronic pain is associated with depression and anxiety-related emotional dysfunction.
In this case, the authors explain that antidepressants that increase the availability of serotonin (a neurotransmitter classically associated with “happiness”) would be the most appropriate in circumstances of neuropathic pain. This is the case with selective serotonin reuptake inhibitors (SSRIs), such as sertraline.
It is essential to have the prescription and continuous medical follow-up since they are not risk-free medications. In addition, in the case of other psychotropics, such as benzodiazepines, their effectiveness has not yet been proven.
Other treatments and measures for sciatic pain
Apart from sciatic nerve pain medications, other measures can be applied. Always with the authorization of the treating professional.
Physiotherapy is recommended to reduce pain, help regain mobility, and prevent the ailment from recurring. Sessions can be carried out in conjunction with the following home techniques:
- Place warm compresses on the area.
- Massage the painful region.
- Do stretching exercises.
- Take natural remedies, such as relaxing infusions.
On the other hand, it is advisable to seek medical attention as soon as possible if the symptoms change abruptly and others appear. These include decreased sensation, weakness or loss of strength, urinary incontinence, and unexplained fever.
The treatment of sciatica is comprehensive
Although patients often receive several treatments throughout their lives (unless the condition resolves), it is convenient that there are several drugs and general measures to alleviate the symptoms.
It is essential to never self-medicate, as these medications have adverse reactions and interactions. A health professional must make the prescription and evaluate the evolution of the pathology.